Prenatal diagnostics
What does prenatal diagnostics mean?
Prenatal diagnostics refers to prenatal examinations that are designed to detect certain diseases or disabilities in the unborn child. These can be performed in different ways and with different risks and accuracies. In Switzerland, major innovations have been made in prenatal diagnostics in recent years. Whereas in the past chromosome testing was only possible invasively and with a risk to the pregnancy, nowadays prenatal diagnostics is in most cases performed non-invasively and thus without a risk to you and your unborn child.
Prenatal diagnostics include prenatal ultrasound examinations, nuchal translucency measurement, first trimester test, NIPT, and chorionic villus sampling and amniocentesis.
Why prenatal diagnostics
93 percent of all children are born healthy. About 7 percent of all children suffer from a disability or malformation. These are often non-threatening problems or those that can be corrected by pediatric surgery.
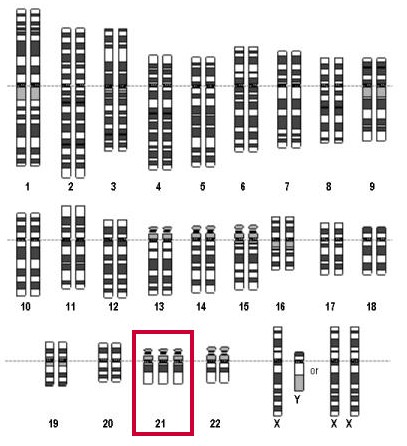
Prenatal diagnostics is about diagnosing the disabilities or malformations at the earliest possible stage of pregnancy. This includes checking the genetic material, the chromosomes of the unborn child. The most common chromosomal disorder is Down syndrome (trisomy 21, formerly known as mongolism), in which there are three copies instead of two of the third smallest chromosome (chromosome 21, marked red in the picture) in each cell nucleus. The frequency of Down syndrome depends strongly on the age of the mother (see table of risk figures).
Risk figures
In the following table you can look up your individual risk for the most common hereditary disorder, trisomy 21 (Down syndrome). The red column shows age, and the column to the left of that shows the risk of a woman of that age giving birth to a child with trisomy 21.
The column to the right of age shows the risk of trisomy 21 if an ultrasound is performed at 11-14 weeks as recommended; this risk is greater than that in the left column because some trisomy children die later in pregnancy.
Example for a 30-year-old woman: risk at birth 1:910, risk at 11-14 weeks 1:415, but with nuchal translucency below 2.5 mm only 1:2075.
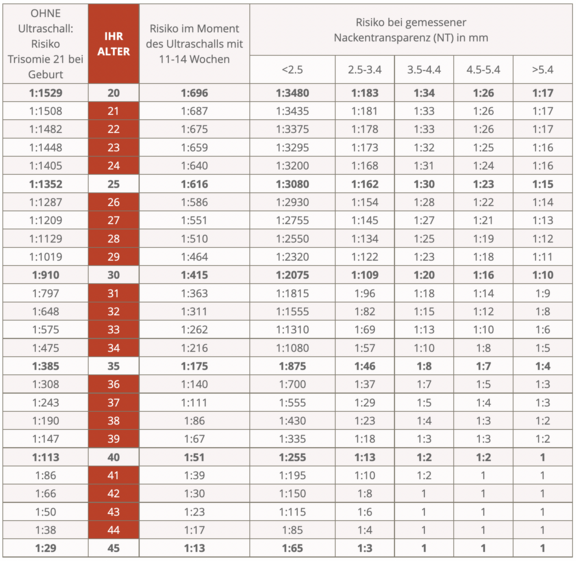
For all mothers together, the risk of trisomy 21 is about 1:700, and the risk of another hereditary disorder is about the same (trisomy 18 1:3000, trisomy 13 1:5000, sex chromosome disorders 1:700). Thus, less than 0.5% of all children have a hereditary disorder, while about 3% have a malformation. The majority of children with malformations thus have a normal genotype.
Which prenatal diagnostics make sense to you?
Our society says yes to prenatal diagnostics on a broad basis, because many parents wonder whether their unborn child will be healthy. However, all examinations (ultrasound, blood tests, amniocentesis, etc.) are completely voluntary.
In our opinion, informed pregnant women should be free to decide which form of prenatal diagnostics they would like to use.
We will discuss which prenatal examinations make sense for you in a detailed consultation in early pregnancy. The father-to-be is cordially invited to attend - as he is to all check-ups. The decisive factor is that, after a comprehensive explanation by your doctor, you have those examinations done that will enable you to look forward to your child without restrictions for the rest of your pregnancy. However, today's prenatal diagnostics cannot give you a guarantee that your child will be healthy.
What prenatal diagnostics do we perform in our practice?
Ultrasound
During your pregnancy check-ups, we can use various methods to assess whether everything is basically okay with the pregnancy or whether there are any risks. Ultrasound is the only method that allows us to directly visualize the unborn child in the uterus.
Safety
Ultrasound (as one of the prenatal diagnostics) is safe; it has been used in pregnancy for almost 40 years, and a large number of studies have never shown a direct harmful effect on the child or mother. With the low sound energies commonly used today, no adverse effects are expected for the expectant child.
Benefits
Ultrasound can be used to answer important questions that are important for the further management of the pregnancy:
In the first trimester, first-trimester test (10-13 weeks), we can determine the integrity and age of the pregnancy. This is of great importance, for example, to be able to detect reduced growth in late pregnancy. Multiple births can also be detected with a high degree of certainty, and we can also detect a number of severe malformations at this early age. By measuring the nuchal skin, we gain information about a possible chromosomal disorder such as Down syndrome (trisomy 21).
In the second trimester, organ screening (20-23 weeks), we assess the baby's growth and amniotic fluid volume, both important indicators of normal development. Important malformations of the head, brain, spine, heart, kidneys, stomach and limbs can be detected. Likewise, the fit of the placenta is assessed because a deep fit or complete covering of the cervix can lead to dangerous bleeding later in pregnancy.
In the third trimester (30-34 weeks), the focus is on fetal growth. A normal-sized baby with normal amniotic fluid levels indicate a functioning placenta. The baby should now have turned in the cranial position to allow for a normal delivery. In addition, some malformations that are important for optimal care of the child after birth can only be detected at this late stage.
Importance of ultrasound
If the ultrasound findings are normal, there is a high probability that everything is fine with your child. However, it is not possible to guarantee a perfectly healthy child. Ultrasound is very good (90% accuracy) at detecting very severe fetal problems that may not allow the child to survive. Ultrasound is fairly good (75% accuracy) at detecting problems that require intensive care and therapy. However, ultrasound is more moderately useful (30% accuracy) for detecting minor malformations such as supernumerary fingers or small, usually insignificant heart defects.
A normal ultrasound finding has an impact on the further management of the pregnancy and can also give you great reassurance. If a problem is detected, the ultrasound can provide us with important information on which to base decisions; you may be able to prepare for the birth of a sick child, the birth can be planned at a center suitable for that purpose, and occasionally a sick child can be effectively treated during pregnancy.
Routine ultrasounds at 10-13 and 20-23 weeks, as well as other ultrasounds on indication (i.e., when there are risks or suspicions), are covered by health insurance.
The ultrasound is a prenatal examination in the sense of the Law on Human Genetic Testing. Depending on the results of the ultrasound, follow-up examinations such as amniocentesis may be indicated. An unexpected result or evidence of a serious fetal disorder could place you in an ethical decision-making conflict ("should I continue the pregnancy or terminate it?"). In prenatal examinations, there is a right not to know, which is why you should let us know if you do not want an ultrasound for personal reasons. If you are unclear or have any questions, we will be happy to provide you with further information, and we can organize independent expert advice for you.
3D/4D ultrasound
Thanks to modern technology, the child can be shown in three dimensions (3D) or in a moving three-dimensional image (4D), while the conventional image shows only a two-dimensional section, such as the profile of the head.
3D/4D ultrasound usually has little diagnostic significance, but is intended to give pleasure to the expectant parents. Our group practice offers the following package, which is not reimbursed by health insurance, for 250 Swiss francs:
- USB stick with Gyné logo (please bring to all consultations);
- 3D/4D images throughout the pregnancy, which are stored on the USB stick. The prerequisite is a favorable position of the unborn child and sufficient amniotic fluid to be able to map the body contours;
- Electronic copy of medical history in PDF format, updated at each consultation (convenient for travel).
Nuchal translucency (NT)
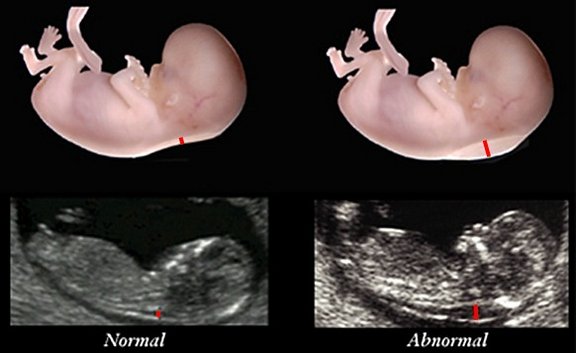
This relatively new indication of a hereditary disorder is checked during ultrasound examination between the 11th and 14th week. The unborn child should be at least 45 millimeters long (crown-rump length). The examination requires experience, a good ultrasound machine and maximum magnification. At this stage of development it is normal if there is a thin fluid cushion in the neck (black stripe, thickness marked by small red line). However, if the nuchal translucency (NT) is thicker than 3.5 millimeters (see right image), this indicates a problem with lymphatic drainage and is suspicious for a genetic disorder or malformation.
Procedure for NT of 2.5 mm and more (5% of pregnant women)
In the case of abnormal NT, further clarification of the genetic material by means of NIPT, amniocentesis or chorionic biopsy is recommended (see next but one chapter). An NT of 2.5 - 3.4 mm corresponds to a gray zone with a slightly increased risk (see table of risk figures), while an NT of 3.5 mm and more (in 1% of all pregnant women) should be clarified in any case.
Prenatal diagnostics by means of first trimester blood test
From the mother's age, nuchal translucency measurement and two blood values, your individual risk for trisomy 21 as well as trisomy 18/13 can be calculated. This is a statistical estimate and not a definitive diagnosis. This blood test is covered by health insurance and is available within a few days.
Measuring NT alone detects about 70% of children with trisomy 21 (Down syndrome), combining it with the first trimester blood test detects between 80% and 85%.
NIPT
Shortly after 2000, the Human Genome Project (HUGO) succeeded in semi-automatically evaluating sections of the human genetic material DNA using so-called massive parallel sequencing, thus decoding the human genome.
Since DNA of the unborn child (so-called cell-free DNA) also circulates in the blood of a pregnant woman, it has been possible since 2012 to deduce the genetic characteristics of the child from a simple blood sample from the 10th week of pregnancy. The effort required for this so-called sequencing is enormous, both in the laboratory and in the computer-assisted evaluation, which is why only specialized laboratories can make the corresponding investments. The procedure is also known as NIPT (non-invasive prenatal testing).
If, after counting millions of fragments, chromosome 21 is overrepresented, this allows us to conclude with a high degree of certainty that the unborn child has three copies instead of two and thus has trisomy 21 (Down syndrome, formerly called mongolism).
Tests offered by our practice
- NIPT from the University of Zurich: based on Illumina® high-throughput sequencing technology:
- Basic Trisomy NIPT (Illumina-VeriSeq® NIPT-Solution): covered by basic insurance under certain conditions for trisomies 13, 18, and 21. This NIPT detects with high probability the most common fetal trisomies 13, 18, and 21, as well as, if desired, variations in the number of sex chromosomes X and Y (e.g., Turner or Klinefelter syndrome), and determination of the child's sex. Cost: 510 CHF.
- Extended NIPT for all visible chromosomal defects (combined Illumina VeriSeq® and internal IMG NIPT): in this combined extension NIPT, all chromosomes (1-22, XY) are examined for trisomies and monosomies as well as for major deletions and duplications. Cost: Additional charge of CHF 350 (not covered by basic insurance).
- In the case of twin pregnancies and egg donation, both tests are also informative.
- Panorama test (Genetica laboratory, Zurich / Natera, California) - examines only particularly significant portions of the chromosomes (SNPs, single nucleotide polymorphisms) and compares them with those of the mother.
- Basic examination: trisomies 21, 18 and 13, triploidy, Turner syndrome. Cost 660.-- Fr. NEW since July 2015: The basic examination is covered by health insurance if the first trimester blood test showed a trisomy risk higher than 1:1000. Otherwise, the supplementary insurance may make a voluntary contribution.
- Supplementary insurance since July 2014: Test for so-called microdeletion syndromes (DiGeorge, Prader-Willi, Angelman, Cri-du-chat, 1p36). Cost additional 250.-- Fr. The five microdeletion syndromes tested are severe and affect a total of one in a thousand newborns. Those who decide to have a new blood test will in the majority of cases also want this additional examination, unless they only want to exclude trisomy 21.
- Also possible in twin pregnancies and pregnancies with donor egg.
Facts and open questions
- An abnormal test result should usually be verified by amniocentesis.
- A NIPT test does not replace detailed ultrasound at 11-14 weeks. In particular, measurement of nuchal translucency (NT, previous chapter) is still useful because this warning sign may indicate problems other than trisomy 21. As a rule, we recommend that the ultrasound with NT measurement be performed first, if only to determine whether the pregnancy is still intact. Only then we will decide together with the pregnant woman how to proceed (conventional first trimester blood test, new paid blood test, directly amniocentesis or no further tests).
- The new blood tests were developed and reviewed for high-risk pregnant women. Young pregnant women with normal nuchal translucency are at such low risk that the new blood test may give almost as many false positives as it detects actual problems. Young pregnant women with normal nuchal translucency are therefore more likely to be recommended to undergo conventional first trimester blood testing - not only because of the cost savings; however, we will always grant the informed request for direct NIPT.
Invasive prenatal diagnostics: amniocentesis, chorionic biopsy
Amniocentesis
Amniocentesis is usually performed between 16 and 18 weeks of pregnancy. A thin needle is used to puncture the amniotic cavity and about 12-15 ml of amniotic fluid is aspirated. The extracted amniotic fluid forms again in a short time. The puncture is performed under ultrasound control, so that injury to the child should not occur today. The risk of miscarriage after amniocentesis is at most 0.5% (1 in 200) and must be weighed against the individual risk of a genetic disorder in the child. Amniocentesis as an invasive prenatal diagnostic method is still considered the gold standard when other non-invasive prenatal diagnostic tests show abnormal results.
Chorionic biopsy
Chorionic biopsy involves the removal of cells from the placenta using a needle. This is possible earlier than amniocentesis (at about 11 weeks); however, the result of the examination is somewhat less reliable than that of amniocentesis, because in rare cases the genetic material of the child and that of the placenta do not match. The examination is particularly suitable for expectant mothers who have already given birth to a sick child.
We do not perform invasive prenatal diagnostics (amniocentesis and chorionic biopsy) ourselves, but refer you to a physician who specializes in this procedure.
Contact
GYNÉ LANG
Kohlrainstrasse 10
8700 Küsnacht (Zurich)
Phone +41 44 912 25 25
praxis@gynelang.ch
Opening hours
| Monday | 08.00 - 12.00 | 13.30 - 16.30 |
| Tuesday | 08.00 - 12.00 | 13.30 - 16.30 |
| Wednesday | 08.00 - 15.00 |
| Thursday | 08.00 - 12.00 | 13.30 - 16.30 |
| Friday | 08.00 - 15.00 |
![[Translate to English:] Frauenarzt Zürich [Translate to English:] Frauenarzt Zürich](/fileadmin/sites/gynelang/media/gynelang_logo.png)