Laparoscopy
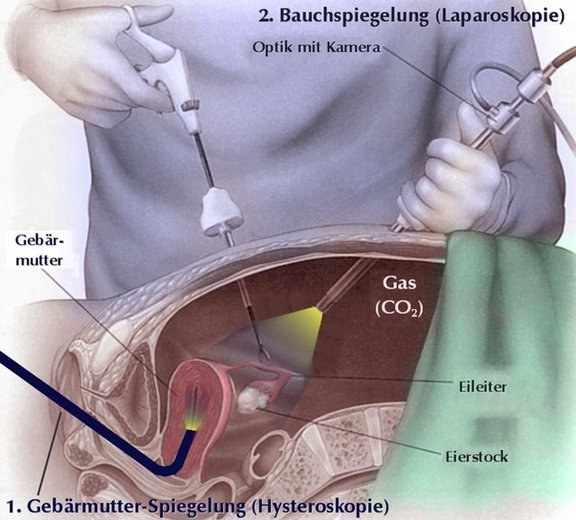
In gynecology, the so-called "buttonhole surgery", laparoscopy, was introduced decades ago. In contrast to the classic operation via an abdominal incision, the operation is performed via small holes in the abdomen. Accordingly, laparoscopy belongs to the so-called minimally invasive surgical technique. Whereas in the past it was possible to look directly into the abdomen via an optical system (laparoscopy means "looking into the abdomen"), today this is done via a camera attached to the optical system, which sends the image to a monitor. This refined method of laparoscopy was like a quantum leap in the history of laparoscopy. Only then did it become possible for more complicated operations to be performed via laparoscopy. A further development was then laparoscopy using robots, where the surgeon sits at a console, away from the patient, and the instruments are guided in real time and in 3D using 2 joysticks.
Robots are used especially for very complex procedures where high precision is required (for example, to protect nerves). The robots themselves are very cost-intensive and the effort required to provide and handle them before and during the operation are also very high. In routine operations such as hysterectomy, no advantage of 3D technology over conventional laparoscopy has been shown so far.
Indications (reasons) for laparoscopy
There are various indications for performing a laparoscopy in gynecology. On the one hand, laparoscopy is the safest method of assessing findings in the abdomen. Endometriosis in particular is a prime example for performing a laparoscopy. Many forms and localizations of endometriosis can only be diagnosed via laparoscopy. The following diagnostic indications may necessitate laparoscopy:
- Clarification of ovarian tumors and cysts
- Clarification in case of desire to have children
- Clarification of the patency of the fallopian tubes
- Clarification of recurrent abdominal pain, in particular
- adhesions of intestine, ovaries, peritoneum etc.
- Detection of tumors or offshoots (metastases) of malignant tumors
- Assessment of the size and location of fibroids on the uterus
Operatively, the following gynecological operations are performed by means of laparoscopy:
- Removal of tumors or cysts of the ovaries or fallopian tubes
- Loosening of adhesions
- Opening of blocked fallopian tubes and formation of new fimbrial funnels
- Removal of fibroids
- Removal and/or vaporization (by CO2 laser) of endometriosis lesions
- Partial or total hysterectomy
- Removal of fallopian tubes or ovaries
- Fixation of the vagina in case of descent problems
- Removal of lymph nodes in the abdomen
- Appendectomy
Performance of laparoscopy
General anesthesia is used to perform a laparoscopy, as the abdominal muscles must be completely relaxed. To obtain the best possible view of the lower abdomen, a bladder catheter is also inserted to drain the urine. Occasionally, a guide instrument must still be inserted into the uterus so that the uterus can be moved to the side during the operation.
On the technical side, an insuflator is needed to pump the gas CO2 into the abdomen, a light source, optics with a camera, and a monitor.
After a stab incision in the belly button, a special needle (Verres needle) is used to probe the abdominal cavity and then the abdomen is filled with CO2 for the subsequent laparoscopy. Now a first working channel, a so-called trocar, is inserted into the abdomen, followed by the camera.
Depending on the operation, 2-4 additional small working channels are inserted into the abdomen under visual control. After a thorough inspection of the abdomen, the actual operation is started. For this purpose, the patient is placed in a head-down position so that the intestines slide towards the upper abdomen, thus exposing the view of the uterus and ovaries.
At the end of the laparoscopy, the air is deflated the trocars are removed and the punctures in the abdomen are closed.
Risks of laparoscopy
Like all surgeries, laparoscopy has its risks. In addition to the risk of bleeding and infection, the main ones are injuries to other organs such as the intestines, bladder or ureters. The risks depend greatly on the operation to be performed during laparoscopy. Overall, however, they are considered rare.
After the laparoscopy, there may be pain in the abdomen and shoulder. This pain usually comes from retained air that accumulates below the diaphragm and irritates the nerve. They are harmless and go away after 24 to 48 hours. The start of bowel movement can also be delayed and therefore unpleasant. For this purpose, laxatives are then administered at an early stage.
Need for hospitalization during laparoscopy
After simpler laparoscopies, the patient can usually leave the hospital the next day. Purely diagnostic laparoscopies can also be performed on an outpatient basis. After more extensive procedures, 2-3 days of hospitalization may be necessary.
What should be observed after laparoscopy?
After a laparoscopy the following general rules apply for 2 weeks
- No bathing, but showering is allowed
- Do not lift heavy weights, maximum 5 kg
- No sports
- No sexual intercourse
Depending on the operation during laparoscopy, further rules of conduct may be added, about which you will be informed before and after the laparoscopy.
Basically, it can be said that the restrictions after laparoscopy are many times less than after open surgery, which is one of the main advantages of this method.
Contact
GYNÉ LANG
Kohlrainstrasse 10
8700 Küsnacht (Zurich)
Phone +41 44 912 25 25
praxis@gynelang.ch
Opening hours
| Monday | 08.00 - 12.00 | 13.30 - 16.30 |
| Tuesday | 08.00 - 12.00 | 13.30 - 16.30 |
| Wednesday | 08.00 - 15.00 |
| Thursday | 08.00 - 12.00 | 13.30 - 16.30 |
| Friday | 08.00 - 15.00 |
![[Translate to English:] Frauenarzt Zürich [Translate to English:] Frauenarzt Zürich](/fileadmin/sites/gynelang/media/gynelang_logo.png)

