Hysterectomy (Uterus removal)
Uterus removal, or hysterectomy, is the last possible step when it comes to definitively solving a problem with the uterus. The decision to have a hysterectomy always wants to be carefully considered. In certain cases it is one of many options (such as for bleeding disorders, fibroids, prolapse, or adenomysis/endometriosis) in other cases, such as for malignant tumors, it is usually the only good method of cure. There are several methods for hysterectomy: from the vagina, through an abdominal incision, or as most commonly performed today, by laparoscopy. The whole subject of hysterectomy is very complex and not infrequently associated with many fears. In the following, we will try to provide some clarity here.
However, an entry on a website about hysterectomy will never be able to replace a personal conversation. This topic is too individual and complex.
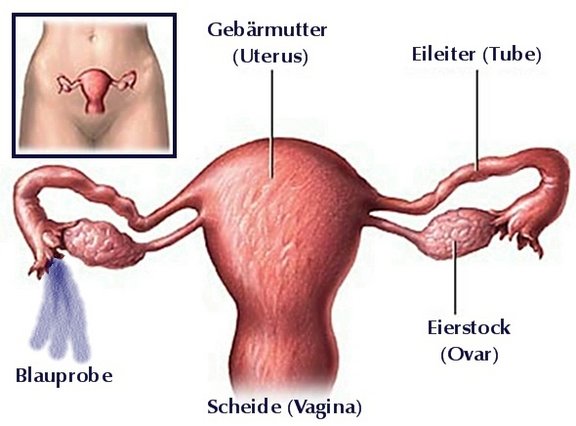
Schematic of the female internal reproductive organs: fibroids and bleeding disorders originate in the body of the uterus (corpus uteri, shaded in red).
Reasons for hysterectomy
Bleeding disorders
Irregular and especially heavy vaginal bleeding, which often leads to anemia or iron deficiency, is a possible reason for hysterectomy. Especially if there is still a desire to have children, all conservative treatment options will be tried first, starting with herbal remedies 8e.g. monk's pepper), to hemostatic medications, to hormones and minor surgical interventions such as uterus endoscopy with removal of polyps or small fibroids. As another alternative to hysterectomy, in special cases it is possible to remove the inner layer of the uterus, the mucosa or endometrium, or to destroy it with heat or laser. These methods also require hospitalization, but the surgery is smaller. It is important to remember with these methods that
- The recurrence rate is about 20%
- Contraception must still be used, but on the other hand
- Pregnancy can no longer be carried to term
- The duration of recovery is similar to that of a laparoscopic partial removal (supracervical hysterectomy, see below)
- The complication rates are comparable to a hysterectomy
- The chances of success in adenomyosis of the uterus (endometriosis in the uterus) are not good.
- It is not suitable for bleeding disorders due to fibroids
Myomas
- Myomas can be quite large (up to the size of a football) and can cause various mechanical problems due to the pressure they exert on the surrounding organs.
- Fortunately, the malignant degeneration of a myoma is very rare.
- If the patient wishes to have a child, we try to avoid hysterectomy whenever possible and remove only those fibroids that are necessary to maintain fertility.
- Often the uterus is riddled with many fibroid nodules. Hysterectomy is then (still assuming that there is no longer a desire to have children) often the less invasive or costly operation than removal of individual nodes.
- After hysterectomy, the problem of fibroids is solved, which can be particularly useful with regard to subsequent hormone replacement therapy.
- Minimally invasive methods should also be mentioned, in which the myoma nodes are attempted to be destroyed by means of ultrasound, heat or occlusion of afferent vessels. We do not actively recommend these methods, as many women experience massive pain after the operation and the risk of having to undergo the procedure several times is relatively high. Even after these methods it is necessary to use contraception. Unfortunately, to this day they are not approved even for women who still want to become pregnant because of the risk of complications during pregnancy.
Uterine prolapse as a reason for hysterectomy
- Uterine prolapse usually occurs as a result of previous births (the larger the children, the more births and the more frequent vacuum or forceps delivery, the more frequent prolapse). It usually occurs together with a descent of the bladder or rectum.
- Removal from the vagina, called vaginal hysterectomy, is usually the procedure of choice here (see below).
Tumors, cancer as a cause for hysterectomy
- In the case of a malignant tumor of the uterus, in the vast majority of cases there is no way around a hysterectomy in order to achieve a cure.
- Depending on the location of the tumor, the extent and involvement of lymph nodes or other organs, the hysterectomy is planned individually.
Total hysterectomy or only partial hysterectomy?
Whereas until about 20 years ago in the vast majority of cases the entire uterus was removed during a hysterectomy, today supracervical hysterectomy, i.e. partial removal of the uterus without the cervix, is often performed if this makes medical sense.
Reasons for a total hysterectomy
- For descent surgery from the vagina, the entire uterus must always be removed for technical reasons. (In certain cases, there is also the possibility of performing descent surgery via laparoscopy, without or with partial removal of the uterus.)
- In case of cancer or premalignant changes of the cervix (cervical dysplasia or cervical carcinoma).
- In case of cancer of the body of the uterus (so-called corpus carcinoma).
Reasons for partial hysterectomy
- Bleeding problems
- Myomas
- Adenomyosis / endometriosis
Advantages of total hysterectomy
- The cervix as a potentially dangerous site for malignant degeneration (cancer) of the cervix is definitely removed, thus the danger is eliminated.
- The periodic preventive smears (PAP smear) no longer need to be performed.
Advantages of the partial removal of the uterus
The cervix is anatomically located in the middle of the pelvic floor, it pierces it, so to speak. In supracervical hysterectomy, the uterus is placed above the neck, i.e. above the cervix (supracervical) and thus above the pelvic floor. The pelvic floor with its fine muscle network, vessels and nerves is not damaged and therefore does not need to be reattached. For this reason, this operation:
- Less traumatic for the pelvic floor
- Less painful after the operation
- With fewer complications
- Associated with a significantly shorter recovery time after surgery (about 2 weeks versus 4-6 weeks after a total hysterectomy).
- Some studies also claim to have shown that sexual intercourse impairment is less common after this surgical technique than after total hysterectomy. However, other studies show that there is no difference after 6-12 months.
How is a hysterectomy performed
There are 3 ways for uterus removal:
Hysterectomy via laparoscopy:
- Most common form of hysterectomy today because it is least invasive and there is shorter convalescence (recovery).
- Laparoscopic (via laparoscopy) total as well as partial hysterectomy is possible.
- Hospitalization 2-3 days
Hysterectomy from the vagina
- Preferred for descent symptoms
- No scars on the abdomen
- Convalescence comparable to surgery via abdominal incision
- Hospitalization 2-3 days
Hysterectomy via abdominal incision
- For very large fibroids
- In case of cancer
- Hospitalization 4-5 days
Which way is the best, must always be decided individually after exact evaluation together. The operation is then explained in detail by means of an operation protocol:
- Information protocol Uterus removal by laparoscopy
- Protocol of hysterectomy from the vagina
- Protocol of uterus removal by abdominal surgery
What happens to the ovaries and fallopian tubes?
If the ovaries still produce hormones (and they do long after menopause) and do not show any pathological changes, we recommend leaving the ovaries in place during hysterectomy.
The situation is different with the fallopian tubes: They do not produce hormones and the woman does not notice the difference whether the fallopian tubes are still present or not. However, we now know that the fallopian tubes are responsible for 80% of malignant ovarian cancers. Therefore, if the fallopian tubes are removed, a significant reduction in the risk of ovarian cancer can be achieved without loss of hormone production or well-being.
Are there any negative effects of hysterectomy such as weight gain or premature aging?
The uterus is a great organ, as it directly enables the development of a child up to birth. However, it does not produce hormones, which is why there are no effects of hysterectomy such as weight gain or premature aging (provided the ovaries are left in place!). What is clear, however, is that with hysterectomy there is no longer the possibility of carrying a child to term. Therefore, the most important question to ask before a hysterectomy is, " Do I want to possibly get pregnant again?" Only if this question can be answered unequivocally with no, a hysterectomy is a good method for benign disorders. Unfortunately, for malignant diagnoses, there is often no alternative to hysterectomy, as survival would be acutely threatened.
Uterus removal book recommendation
The decision whether to remove the uterus is often not easy and many questions may arise. Of course, we will be happy to answer these questions in a detailed consultation and accompany you on this decision-making process. However, you may also find this book, written by an affected woman, helpful: "Meine (Ex) Gemärmutter".
Contact
GYNÉ LANG
Kohlrainstrasse 10
8700 Küsnacht (Zurich)
Phone +41 44 912 25 25
praxis@gynelang.ch
Opening hours
| Monday | 08.00 - 12.00 | 13.30 - 16.30 |
| Tuesday | 08.00 - 12.00 | 13.30 - 16.30 |
| Wednesday | 08.00 - 15.00 |
| Thursday | 08.00 - 12.00 | 13.30 - 16.30 |
| Friday | 08.00 - 15.00 |
![[Translate to English:] Frauenarzt Zürich [Translate to English:] Frauenarzt Zürich](/fileadmin/sites/gynelang/media/gynelang_logo.png)

